Epidural steroid injections (ESIs) are a common go-to for managing chronic back pain, sciatica, and lumbar disc issues. These injections are widely used in pain clinics and spine care centers across the globe. However, despite their popularity and short-term effectiveness, there’s a lesser-discussed aspect that deserves attention—the dark side of epidural steroid injection.
In this guide, we’ll explore what these injections are, how they work, and more importantly, the hidden risks and long-term side effects you need to be aware of before considering this form of treatment.
What Is an Epidural Steroid Injection?
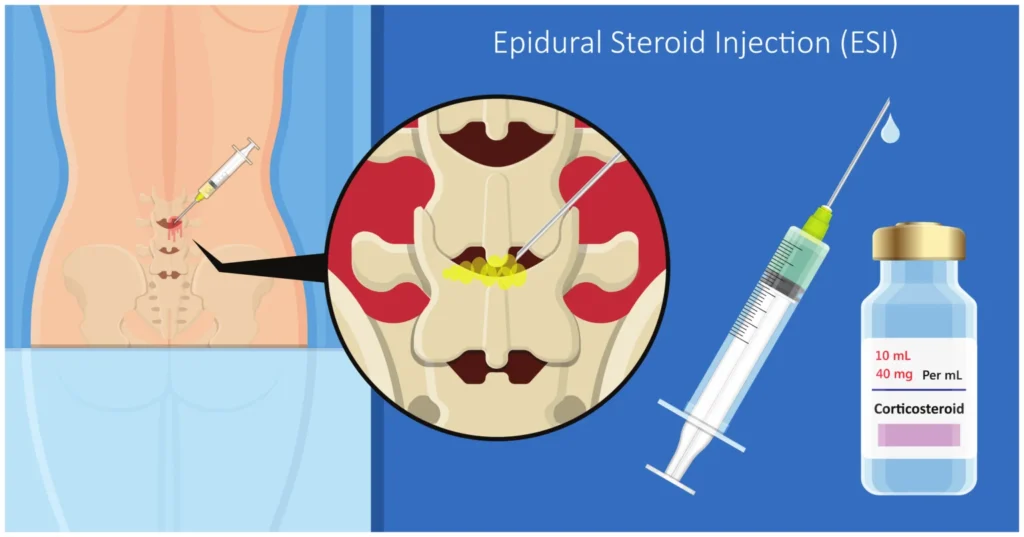
An epidural steroid injection involves delivering a corticosteroid (usually mixed with an anesthetic) into the epidural space around your spinal cord. The goal is to reduce inflammation and provide relief from conditions like:
- Herniated or bulging discs
- Sciatica
- Spinal stenosis
- Degenerative disc disease
According to the Mayo Clinic, epidural steroid injections are often used when physical therapy and oral medications fail. This treatment is often considered when oral medications, physical therapy, and conservative approaches fail to manage persistent back or leg pain.
Types of Epidural Injections
- Lumbar Epidural: Targets lower back pain, often at L4-L5 or L5-S1 levels.
- Transforaminal Epidural Steroid Injection: Focuses on specific nerve roots for conditions like sciatica.
- Caudal Epidural: Administered at the base of the spine, ideal for widespread lower back pain.
Common Injection Sites for Back Pain
The lower spine is one of the most frequent targets for these injections, particularly in the lumbar region.
L4-L5 Lumbar Epidural Steroid Injection
This site is commonly chosen for disc herniation and nerve root compression. The L4-L5 level supports a significant portion of the spine’s load, making it a hotspot for pain.
L5-S1 Epidural Steroid Injection
The L5-S1 level is associated with sciatic nerve pain, affecting the buttocks, legs, and feet. Injecting here can bring temporary relief for patients with radiating pain.
Both of these locations can be targeted via transforaminal, interlaminar, or caudal approaches, depending on the physician’s assessment.
How Does an Epidural Steroid Injection Work?
The epidural steroid injection procedure involves a needle delivering a corticosteroid (like cortisone) and a local anesthetic into the epidural space. Using fluoroscopy or ultrasound for precision, the injection reduces nerve inflammation caused by conditions like a herniated disc or spinal stenosis. The process takes 15-30 minutes, with patients often feeling relief within days.
What to Expect During the Procedure
- Injection: A combination of steroids and anesthetic is delivered, sometimes causing brief discomfort.
- Preparation: You’ll lie face-down, and the injection site is sterilized.
- Imaging Guidance: Ensures the epidural needle targets the correct spinal level.
Short-Term Benefits of Epidural Injections
For many, the relief is almost immediate. Benefits include:
- Reduced nerve inflammation
- Improved mobility
- Decreased dependency on oral painkillers
Patients experiencing acute flare-ups often report pain reduction within 48–72 hours post-injection. These back injections for pain are sometimes repeated in intervals of 3–4 months.
Common Side Effects of Epidural Steroid Injections
While many tolerate ESIs well, the epidural steroid injection side effects can range from mild to disruptive. Understanding these is crucial before opting for a cortisone shot in back.
Short-Term Side Effects

- Injection Site Pain: Soreness or bruising at the injection site, lasting 1-2 days.
- Facial Flushing: A warm, red face due to steroid effects, typically resolving within 48 hours.
- Blood Sugar Spikes: Temporary increases, a concern for diabetic patients.
- Headaches: Caused by minor pressure changes in the spinal canal.
- Insomnia or Anxiety: Steroids may cause restlessness or mood changes for a few days.
These effects are usually temporary but can be bothersome, especially for those receiving back injections for pain. Cleveland Clinic highlights these side effects as common but typically short-lived
The Dark Side: Serious Risks of Epidural Steroid Injections
The dark side of epidural steroid injection lies in its potential for rare but severe complications. While ESIs are generally safe when performed by skilled professionals, the following risks highlight why caution is warranted.
Infections
Infections, though rare (less than 1% of cases), are a serious concern.
- Epidural Abscess: A bacterial infection in the epidural space, causing fever, pain, or neurological issues.
- Meningitis: Inflammation of the spinal cord’s protective layers, potentially life-threatening.
- Prevention: Sterile techniques and experienced providers reduce this risk.
Nerve Damage
Improper needle placement during a spinal injection can injure nerves, leading to:
- Numbness or Tingling: Temporary or, in rare cases, permanent sensory changes.
- Weakness: Muscle weakness in the legs or arms if nerves are affected.
- Risk Factors: Inexperienced providers or lack of imaging guidance increase this risk.
Spinal Headaches
A puncture in the dura (the spinal cord’s protective membrane) can cause a cerebrospinal fluid leak, leading to:
- Post-Dural Puncture Headache: Severe headaches worsened by sitting or standing.
- Treatment: Rest, hydration, or a blood patch procedure to seal the leak.
Hormonal Imbalances
Repeated steroid injections for back pain can disrupt the body’s natural hormone production.
- Adrenal Suppression: Reduced cortisol production, leading to fatigue or weakness.
- Weight Gain or Mood Changes: Steroid overuse may cause metabolic shifts.
Bone Weakening
Frequent cortisone shots in back can weaken bones over time.
- Osteoporosis Risk: Increased with multiple injections, especially in older adults.
- Fracture Risk: Weakened vertebrae may lead to spinal fractures.
Allergic Reactions
Though rare, some patients react to steroids or contrast dye used during the procedure.
- Symptoms: Rash, itching, or, in severe cases, anaphylaxis.
- Prevention: Disclose allergies to your doctor beforehand.
Long-Term Concerns with Repeated Epidural Injections
The dark side of epidural steroid injection becomes more pronounced with repeated use. Guidelines typically limit ESIs to 3-4 per year to minimize risks.
Weakened Spinal Tissues
- Cartilage Damage: Steroids may degrade spinal cartilage, worsening conditions like degenerative disc disease.
- Ligament Weakening: Prolonged exposure can affect spinal stability.
Reduced Effectiveness
- Diminishing Returns: Pain relief may lessen with each subsequent injection.
- Dependency Risk: Patients may rely on injections instead of addressing underlying causes.
Systemic Effects
- Hormonal Disruption: Long-term steroid use can affect metabolism, bone density, and immune function.
- Increased Pain: Some patients report worsening pain after repeated injections.
L4-L5 and L5 Epidural Injection Side Effects
Side effects may vary depending on the injection site:
L4-L5 Lumbar Epidural Steroid Injection Side Effects:
- Lower limb weakness
- Radiating pain if the nerve root is irritated
- Limited mobility post-injection
L5 Epidural Steroid Injection Side Effects:
- Sciatic flare-up
- Tingling or numbness down the leg
- Discomfort while walking or sitting
Always report site-specific symptoms to your healthcare provider, especially if they persist beyond a few days.
Epidural for Sciatica and Nerve Pain: A Closer Look
Epidural injections are often used to relieve sciatic nerve pain, especially in the L5-S1 region.
While many report improvement, some patients experience:
- Only temporary relief, lasting a few weeks to months
- Rebound inflammation once the steroid wears off
- Dependency on repeat injections
This raises ethical and clinical concerns about overuse without addressing the root cause.
Are Epidural Steroid Injections Overused?
According to data from pain clinics and spine centers, steroid injections for back pain have become increasingly common—even in patients with conditions where they offer minimal long-term benefit.
Many experts argue that this treatment is sometimes offered as a quick fix rather than part of a comprehensive recovery plan, contributing to overreliance and risk exposure.
A 2011 NIH study found limited long-term effectiveness and noted a rise in unnecessary use
Minimizing Risks During Epidural Steroid Injections
To reduce the dark side of epidural steroid injection, take these precautions.
Choose a Qualified Provider
- Opt for board-certified pain specialists or anesthesiologists with extensive ESI experience.
- Ensure the facility uses sterile techniques and modern imaging (fluoroscopy or ultrasound).
Pre-Procedure Preparation
- Disclose medical history, including diabetes, allergies, or past reactions to steroids.
- Avoid blood thinners (as advised by your doctor) to reduce bleeding risk.
Post-Procedure Monitoring
- Watch for signs of complications: fever, severe headaches, or neurological changes.
- Report persistent pain or swelling to your doctor immediately.
Exploring Safer Alternatives to Epidural Injections
If you’re considering other options, here are viable alternatives:
Physical Therapy
Focused exercises can strengthen core muscles and reduce spinal pressure.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
These may help reduce inflammation without the risks of steroids.
Nerve Blocks
An alternative to corticosteroid injections, nerve blocks can interrupt pain signals temporarily.
Acupuncture and Chiropractic Care
Some patients find relief through these non-invasive approaches.
Surgical Intervention
In severe cases, surgical correction may be the only long-term solution.
Who Should Avoid Epidural Steroid Injections?
These injections may not be safe for individuals with:
- Diabetes (due to steroid-induced blood sugar spikes)
- Severe osteoporosis
- Bleeding disorders
- Infections or compromised immunity
Consult a physician who specializes in spinal injection procedures before proceeding.
Frequently Asked Questions (FAQs)
Final Thoughts: Weighing the Risks and Benefits
While epidural steroid injections can offer short-term relief, the dark side of epidural steroid injection lies in its potential for serious side effects and dependency. These spinal injections should not be your first or only solution for back pain. Always pursue comprehensive treatment options, and make informed decisions with your healthcare provider.
The truth about epidural steroid injections isn’t that they don’t work—it’s that they must be used with caution. Being fully informed helps you weigh the risks and benefits for your unique situation.
Disclaimer: The content on Wellness Derive is for informational purposes only and not a substitute for professional medical advice, diagnosis, or treatment. Always consult a healthcare provider for medical concerns.